Your Injury
- Abdominal Injuries
- Achilles Tendon Injuries
- Ankle Injuries
- Back Pain Lumbar Spine (Low)
- Back Pain Thoracic Spine (Middle)
- Buttock Pain
- Calf Pain
- Elbow Pain
- Foot Pain
- Groin Injuries
- Hamstring Injury
- Hand and Finger Injuries
- Headache
- Hip Pain
- Knee Injuries and Knee Pain
- Neck Pain
- Numbness, Tingling and Nerve Pain
- Thigh (Quadricep) Injuries
- Sciatica
- Shoulder
- Shoulder Blade (Scapula) Pain
- Toe Pain
- Wrist Injuries
Knee Injuries and Knee Pain
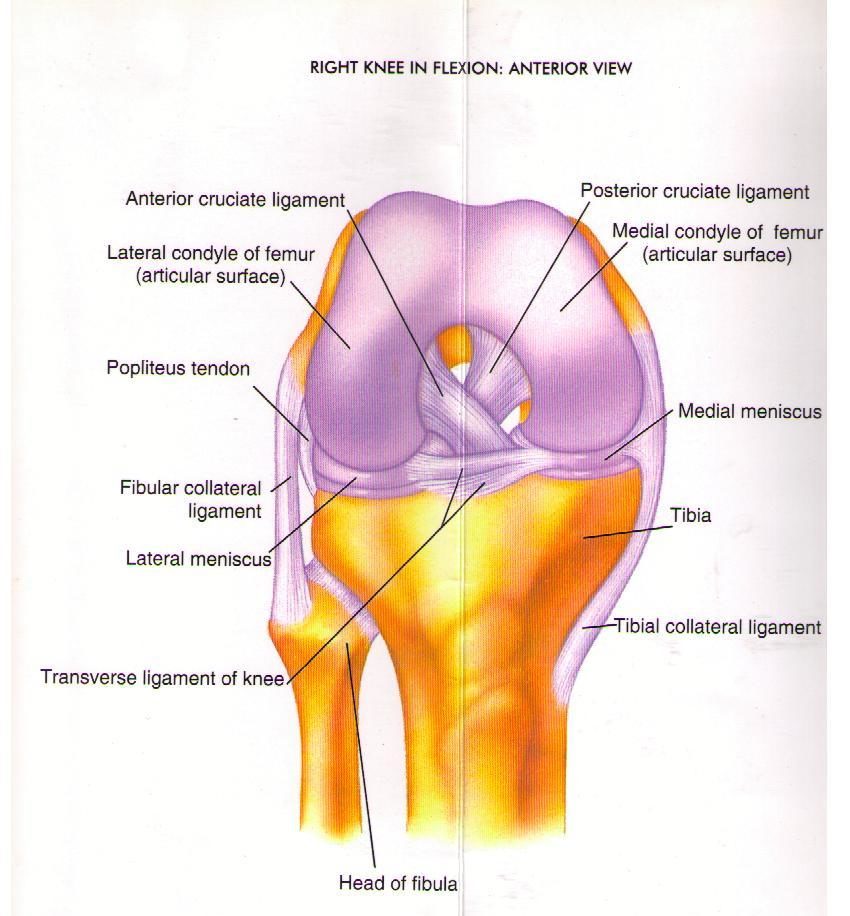
Knee injuries and knee pain can result from disruption of any structures of the knee itself or from referral of another unrelated region. Neck pain is commonly caused by the cervical spine, muscles, ligaments, and soft tissues of surrounding areas The knee joint is made up of four bones, which are connected by muscles, ligaments, and tendons. The fibula is the smaller, outside bone in the lower leg. The Tibia is the front, shin bone. The patella or knee cap, is the small bone in the front of the knee. It slides up and down in a groove in the femur (the femoral groove) as the knee bends and straightens. Common knee injuries include sprains and strains, generalized knee pain, ligament damage, and structural changes. All of these knee injuries can be managed and treated by your physiotherapist.
There are a number of different things that can cause knee pain, of which we will consider the most common in further detail:
Anterior Cruciate Ligament (ACL) tear/rupture
What is an ACL tear?
The ACL is a primary stabilizer of the knee. It limits rotation and forward translation of the joint on itself.
What causes an ACL tear?
Tears of the ACL are quite common, particularly in sports people or people participating in ractivities involving twisting and turning forces about the knee e.g skiing. ACL tears mainly occur in a non contact situations, usually when the person lands awkwardly from a jump whilst twisting or pivoting, or coming to a halt suddenly.
How does an ACL tear feel?
The person will often describe an audible pop or crack, or the feeling of something ‘going out then coming back in’. Most complete tears of this ligament are exceptionally painful, especially in the first few minutes after injury. Straight after the injury it is almost impossible to continue activity. After some time the athlete may attempt to return to play but will often then have an acute episode of instability or giving way. There is limited movement, loss of ability to straighten the knees well as generalised knee pain.
Management of an ACL tear and how to fix it
You will need to see your physiotherapist so they can assess the extent of the tear. You may then be referred to a specialist such as a sports physician or orthopaedic surgeon. Depending on your levels of activity and the extent of the damage, surgical repair (or knee reconstruction) will more than likely be the next option. Before and after surgery it is highly recommended to undergo physiotherapy rehab to best return normal function through stretching, strengthening of the muscles of the leg and pelvis/core and to gradually retrain sporting or work specific tasks. Typically, return to sport is a minimum of 6 months following surgery. Appropriate surgery and rehabilitation will in most cases return you to your pre injury level of activity. The PEP Program (Prevent injury and Enhance Performance) is a series of exercise drills designed to prepare people to return to sport and has been shown to reduce the incidence of re-injury.
Meniscal tear
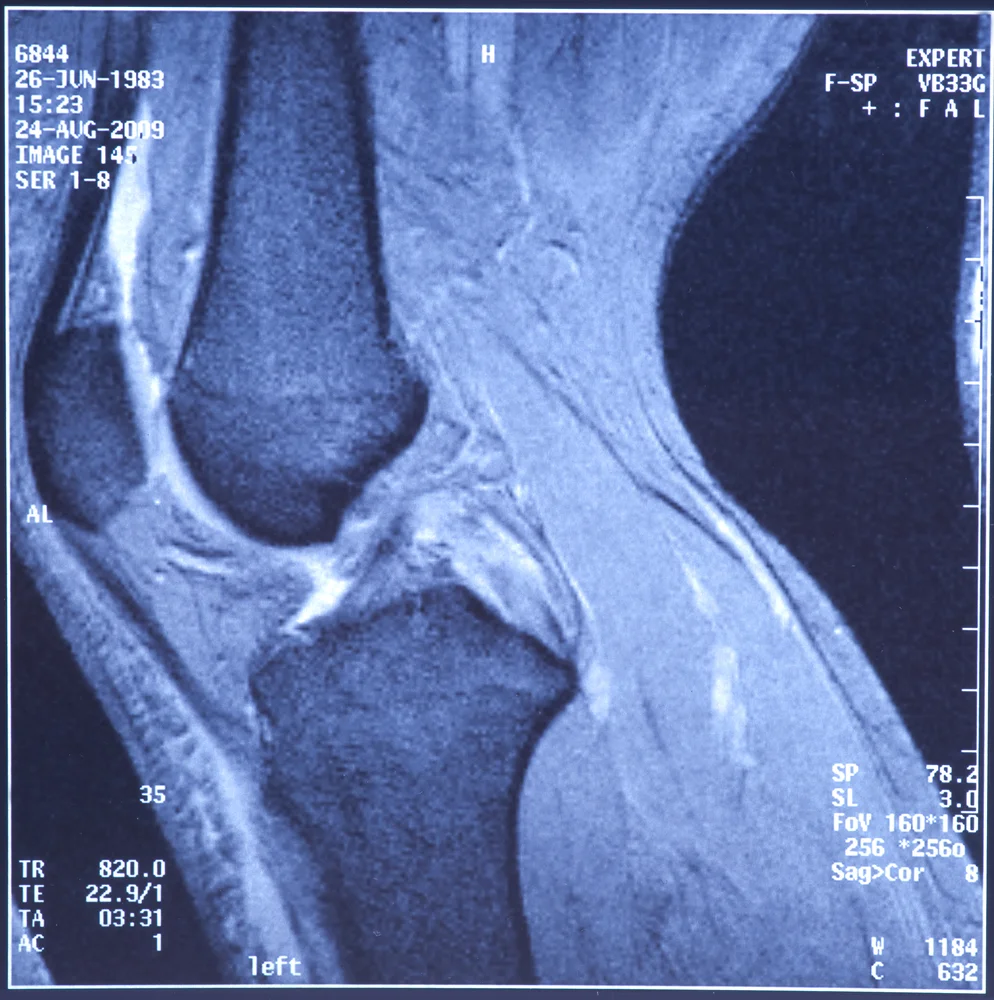
What is a meniscal tear?
The meniscus is best described as the shock absorber inside the knee joint. There are two meniscii, medial and lateral. They sit between the two bones that comprise the knee joint. The knee is the largest joint in the body so the meniscii plays an important role in support and cushioning.
What causes a meniscal tear?
The most common way to tear the meniscus is a twisting injury with the foot anchored to the ground. However, meniscal degeneration can also occur over time if the person has a history of sports with high impact on the knee joint and that involve a high degree of twisting, for example netball.
How does a meniscal tear feel?
The amount of pain associated with an acute meniscal injury varies quite markedly. Some people may describe a tearing sensation. A small tear may cause no immediate pain, but may become painful and swell over the next day or so. People who experience a severe tear may notice more extreme symptoms. Pain and restriction of movement may occur soon after the injury. Generally people with meniscal injuries will describe pain along the joint lines of the knee, locking sensations periodically, and a diffuse pain that is hard to pinpoint to one spot. There is usually a restricted range of motion particularly into knee flexion (bending of the knee is difficult).
Management of a meniscal tear and how to fix it
The management of meniscal injuries varies depending on the severity of the tear. Very small, peripheral tears can be treated conservatively with physiotherapy. Large tears which cause locking and pain will require surgery. Surgery is performed through an arthroscope, where the torn part of the meniscus is removed or repaired. Physiotherapy is required before and after surgery to strengthen the muscles around the joint and to increase range of movement in the knee. Functional strengthening and conditioning is part of a good rehabilitation program.
Patella tendonopathy (tendonitis)
What is patella tendinopathy?
Patella tendinopathy was first known as ‘jumpers knee’. It describes pain underneath the knee cap just above the top of the shin. The pain is usually made worse by jumping, bending, hopping and bouncing.
What causes patella tendinopathy?
This is usually caused by changes in the patella tendon which attaches to the bottom of the kneecap. Factors that make this worse can be poor quadriceps strength and poor lower limb biomechanics. It is an overuse injury caused by loads which are excessive and so not enabling the tendon to adapt quickly enough to stress being placed on it.
How does patella tendinopathy feel?
The patient complains of pain in the area over the tendon, directly under the kneecap. There can also be swelling and spots of extreme local tenderness. On examination the tendon can feel thickened. Pain is increased with activities such as climbing and descending stairs, squatting and crouching.
Management of patella tendinopathy and how to fix it
Usually this condition can ma managed conservatively by physiotherapy. Your physio will set up an appropriate rehabilitation program involving stretching, strengthening exercises, RICE (rest, ice, compression, elevation), proprioception and balance exercises. A biomechanical assessment will be necessary to minimize the risk of injury again.
Patello-Femoral (Knee Cap) Pain
What is Patellofemoral Pain /Anterior Knee Pain ?
Anterior knee pain is usually attributed to “patellofemoral” pain: the joint between the patella (knee cap) and the end of the femur (thigh bone).
The pain is typically experienced over the front of the knee or feels like it could be under the kneecap. The pain worsens with running or walking, particularly down hills or with descending stairs.
What causes it?
There may be several things that can contribute, including:
- Sudden increase or change in training/exercising
- Activities that load the knee cap excessively e.g squats/lunges, stairs or kneeling
- Overpronating feet
- Hip/glutes weakness (especially in females)
- Hip control – meaning control your thigh/knee during a landing or squat, as it often turns excessively inward
How does Patello-femoral pain feel?
- Typically, you will feel a deep ache which increases when you increase load on the knee.This could occur with running, jumping, kneeling and use of stairs
- Pain can also occur when the knee is held in a bent position e.g sitting. It is also know as ‘Movie-goers knee, ’ for this reason
- Occasionally the knee will swell and feel stiff
Management of Patello-femoral pain and how to fix it:
Depending on the assessment findings, treatment could entail any or all of:
- VMO (inner quadriceps) strengthening including the timing of activity with respect to lateral quadriceps muscles
- Hip strengthening exercises (clams, bridges, squats, leg press, hip abduction)
- Hip control exercises (single leg squats, step ups, step downs)
- Shortening your stride and increasing your step rate
- Stretching of tight surrounding structures (including hamstring and ITB)
- Foam roller massage
- Consideration to footwear mechanics
ITB Friction Syndrome
What is ITB pain or ITB Syndrome?
The ITB (Iliotibial Band) runs from your ilium (outer hip/pelvic bone) down to your tibia (shin bone). It wraps over the muscle on the outer aspect of your thigh.
Pain can develop on the outer aspect of the knee where the ITB crosses over the end of the femur (thigh bone).
The main difference between ITB syndrome and Patellofemoral syndrome is the location of the pain, as they share some of the causes and treatments. ITB friction worsens with walking, running, and maintaining a slight bend in the knee.
What causes it?
There may be several things that can contribute, including:
- Tightness in the ITB
- Sudden increase in training/exercising
- Hip/glutes weakness, particularly gluteus medius. This leads to greater tension being placed on the ITB
- Hip control – meaning control your thigh/knee during a landing or squat, as it often turns excessively inward
How does ITB friction feel?
- A sharp pain is felt on the outside of the knee with activities involving repeated bending of the knee joint. This can become a constant ache when the irritation increases
Management of ITB Friction and how to fix it:
Depending on the assessment findings, treatment could entail any or all of:
- Hip strengthening exercises (clams, bridges, squats, leg press, hip abduction)
- Hip control exercises (single leg squats, step ups, step downs)
- Shortening your stride and increasing your step rate
- Stretching
- Foam roller massage of the ITB
- Footwear mechanics considerations